Abstract
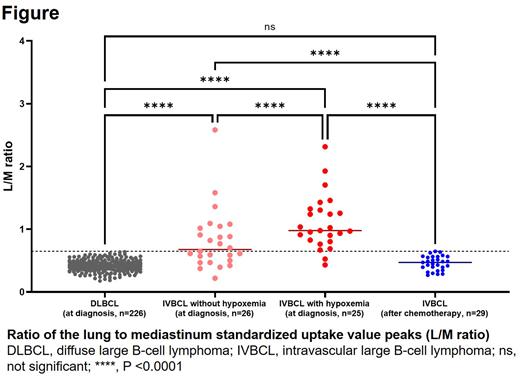
[Introduction] Intravascular large B-cell lymphoma (IVBCL) is a rare subtype of extra-nodal diffuse large B-cell lymphoma (DLBCL), characterized by preferential growth of lymphoma cells within the lumina of small vessels. Clinical presentation of IVBCL is highly variable, and it often includes organ dysfunction related to obstruction of blood vessels. Up to 80% of IVBCL cases experienced hypoxemia at initial presentation, suggesting a high rate of respiratory involvement. In recent years, some IVBCL cases with diffuse pulmonary uptake on 18F-fluorodeoxyglucose (FDG) PET/CT have been reported from Asia and Western countries. It may also reflect the pulmonary infiltration of IVBCL; however, there are no reports of detailed studies with a large number of IVBCL cases. [Methods] We retrospectively evaluated patients with histopathologically proven newly diagnosed IVBCL according to the 2008 World Health Organization criteria between January 2010 through February 2022 from hospitals participating in the North Japan Hematology Study Group (NJHSG). PET/CT images were reviewed by an experienced nuclear medicine physician (S.W.). In addition to the general PET/CT evaluation, the ratio of the lung to mediastinum standardized uptake value (SUV) peaks (L/M ratio) was calculated to assess the degree of FDG accumulation in the lungs objectively. Lung SUV peaks were measured uniformly about 1 cm medial to the right lower lobe pleura, and mediastinum SUV peaks were measured in the left atrium. The L/M ratio of 226 advanced stage DLBCL cases diagnosed within the same periods was also calculated and compared with IVBCL cases. [Results] We identified fifty-one IVBCL patients (age 30-89 years, median 65 years; 56.9% male) who performed PET/CT at diagnosis, and 29 of whom also underwent after chemotherapy. IVBCL was diagnosed via skin biopsy in 31 (60.8%) cases, bone marrow biopsy in 15 (29.4%) cases, and lung biopsy in 8 (15.7%) cases. Hypoxemia were observed in 25 (49.0%) patients. Twenty-eight (54.9%) patients had poor performance status (ECOG score ≥2). Elevated LDH level was observed in 48 (94.1%) cases (median, 631 IU/L; range, 147-4907 IU/L). Diffusely elevated FDG uptake was seen at the lung in 28 (54.9%) patients, bone marrow in 40 (78.4%), and spleen in 32 (62.7%). Chest CT evaluation revealed that ground-glass opacity lesion corresponding to the areas of FDG accumulation on PET was observed in 14 of 28 patients. At diagnosis, the median L/M ratio was significantly higher in IVBCL patients than in DLBCL patients (IVBCL: median, 0.903; range, 0.22-2.583 vs. DLBCL: median, 0.421; range, 0.177-0.639, P < 0.0001, Fig.). ROC analysis revealed that the cutoff value of the L/M ratio of 0.649 predict IVBCL diagnosis. Area under curve was 0.916 (95% CI: 0.859-0.974). Thus, we classified patients with a threshold of 0.649 for the definition of "high” or "low” levels of the L/M ratio. At the time of diagnosis, 38 of 51 (74.5%) IVBCL cases were classified as having a high L/M ratio. The L/M ratio decreased to low levels in all patients who underwent FDG PET/CT after chemotherapy (median, 0.471; range, 0.269-0.647, Fig.). The high L/M ratio was significantly correlated with diffuse FDG uptake in the lung (P < 0.0001), bone marrow (P = 0.0507) and spleen (P < 0.001) and the presence of hypoxemia (P < 0.01). Surprisingly, 14 of 26 (53.8%) patients who did not present with hypoxemia showed high L/M ratio. Fifty (98%) patients received rituximab-containing chemotherapy. Of the patients treated, 13 (26%) patients experienced a relapse, and 9 (18%) patients eventually died. The 2-year overall survival (OS) was 84.6 % (range, 70.3-92.4 months). Median follow-up duration was 48.8 months (range, 4.7-140.5 months) in survivors. The L/M ratio did not stratify the prognosis significantly (L/M high: 2-year OS, 82.3%; 95% CI, 64.6-91.6 vs L/M low: 2-year OS, 90.9%; 95% CI, 64.6-91.6, P = 0.7). [Conclusion] To our knowledge, this is the largest study to assess pulmonary PET/CT findings in newly diagnosed IVBCL cases. A high L/M ratio was found in about 75% of patients with IVBCL while not in advanced stage DLBCL. Given that the L/M ratio decreased after treatment, the high L/M ratio reflects pulmonary infiltration of lymphoma cells. In cases of suspected IVBCL, FDG-PET can be a good indicator of whether to perform a lung biopsy, even in patients without hypoxemia.
Disclosures
Horiguchi:AbbVie GK: Honoraria; AstraZeneca KK: Honoraria; Janssen Pharmaceutical KK: Honoraria. Teshima:TEIJIN PHARMA: Research Funding; NIPPON SHINYAKU: Research Funding; Luca Science Inc.: Research Funding; Novartis: Membership on an entity's Board of Directors or advisory committees, Other: Manuscript preparation, Research Funding; Janssen: Other: Manuscript preparation; Fuji Pharma: Research Funding; Astellas: Research Funding; Chugai: Research Funding; Bristol-Myers Squibb: Honoraria; Pfizer: Honoraria; Takeda: Honoraria, Membership on an entity's Board of Directors or advisory committees; Merck Sharp & Dohme: Honoraria, Membership on an entity's Board of Directors or advisory committees; Sanofi: Research Funding; Kyowa Kirin: Honoraria, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.